Written by Stephen A. Wilson
From his column To Your Health
Haga clic aquí para ver esto en español
 2023 marks the centennial of the first shipment of commercially made insulin by pharmaceutical manufacturer Eli Lilly. It was a blessing for those suffering from diabetes mellitus—a chronic illness that causes many problems, including vision impairment and death. Over the years, millions of lives have been saved or prolonged thanks to insulin. Still, according to the Centers for Disease Control and Prevention (CDCP), 37.3 million American (1 in 10) have diabetes type 2 (DM2) and 96 million more (1 in 3) have prediabetes. Today, let’s look at the difference between DM1 and DM2, and consider the treatments and behaviors for living with them.
2023 marks the centennial of the first shipment of commercially made insulin by pharmaceutical manufacturer Eli Lilly. It was a blessing for those suffering from diabetes mellitus—a chronic illness that causes many problems, including vision impairment and death. Over the years, millions of lives have been saved or prolonged thanks to insulin. Still, according to the Centers for Disease Control and Prevention (CDCP), 37.3 million American (1 in 10) have diabetes type 2 (DM2) and 96 million more (1 in 3) have prediabetes. Today, let’s look at the difference between DM1 and DM2, and consider the treatments and behaviors for living with them.
Glucose is human fuel. The body uses glucose, amino acids, and fat for energy. It is the brain’s main fuel. The body is designed to keep glucose levels in a consistent range. Food comes in the mouth, moves down the esophagus and into the stomach. There, acids and enzymes digest it, releasing glucose that goes into the small intestines where it is absorbed into the bloodstream. Insulin, then, helps glucose get into the cells, where it is used as fuel for the processes that enable life.
When you eat, glucose in your blood increases. Pancreas beta cells sense this and release insulin to allow muscle, fat, and liver cells to use it. What is not immediately used is stored as glycogen for later. When blood glucose levels drop, beta cells stop producing insulin, and pancreas alpha cells prompt the liver to break down stored glycogen back into glucose.
Diabetes is diagnosed when there is a fasting blood glucose level of more than 125 mg per deciliter, or hemoglobin A1C of 6.5% or higher. An A1C test measures average blood glucose for the past two to three months. DM1 and DM2 are two paths to the same problem—the body becomes unable to properly store and use glucose.
DM1 is a "quantity" problem that results when the immune system attacks beta cells in the pancreas so they no longer make insulin. DM1 is unpreventable and usually diagnosed in children and adolescents.
DM2 is a "quality" problem where the body is not effectively using insulin produced by pancreas beta cells. The pancreas responds to decreased sensitivity to insulin by producing more to keep glucose in the normal range (60 to 125 mg/dl). Eventually, the pancreas becomes damaged and unable to make enough insulin, resulting in hyperglycemia (high blood glucose levels). When sustained for a long time, hyperglycemia damages the blood vessels. This increases risk for heart disease, heart attack, stroke, nerve damage, kidney disease, and an eye disease called retinopathy. As weight goes up, the risk of DM2 goes up. As the number of people with obesity has increased, so has the number of people with DM2.
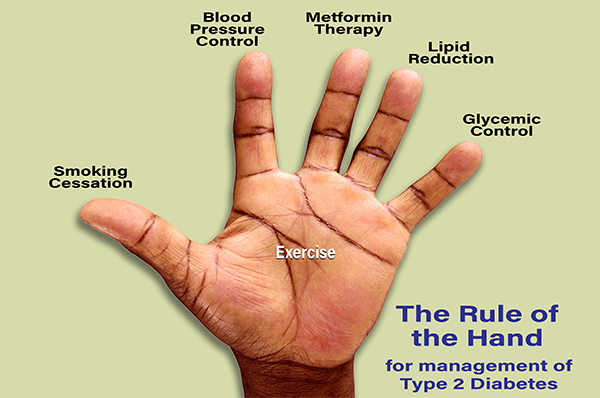
Three things help people with DM2 to lower blood glucose to normal levels: exercise, diet, and medication. Exercise burns fuel, causing increased use of glucose from the blood. Diet results in less glucose in the bloodstream. Both exercise and diet decrease the amount of insulin the body needs and can help make the body more sensitive to the insulin it produces. The DM2 “Rule of the Hand” (see above) is a quick way to help remember these and other things people can do to decrease or delay the effects of diabetes on their bodies.
Medications can force the pancreas to produce more insulin (until it cannot), help the body better utilize or store glucose from the blood, encourage the kidneys to filter out more glucose, or simply be insulin, but that is not enough. The goal is to live longer and better—not just have a normal glucose level.
The three most important behaviors one can take to improve their life with DM2 include exercising more, keeping blood pressure (BP) under 140/90 and stopping smoking, if applicable . Overly tight BP control is not advantageous for most people and, for some, can actually increase the risk of poor outcomes. Because of their beneficial effects on the kidney, either an angiotensin-converting enzyme inhibitor (ACEI) or angiotensin receptor blocker (ARB), should be taken by persons with DM2, unless they are allergic or cannot tolerate them.
The current bedrock medicine for DM2 is metformin. It improves patient outcomes better than other medications. Because of its value, and because it can also cause digestive system side effects, dosing is usually started low, and slowly increased over weeks.
Statins are drugs that lower the level of lipids (fatty compounds) in the blood. Being on statin medication, for example atorvastatin (Lipitor) and rosuvastatin (Crestor), can decrease or delay risk for heart attack, stroke, and kidney disease.
A newer medication group—GLP1 agonists (e.g., semaglutide, liraglutide)—is now being used with metformin. Strong data indicate they improve outcomes beyond lowering glucose levels. Some of the benefit is caused by helping people to lose weight.
Another new group of DM2 medicines is SGLT2 inhibitors. These lower glucose levels by prompting the kidneys to remove sugar from the bloodstream though urination.
There are many other medicines for DM2, including insulin, but those approaching or with DM2 should keep in mind that behaviors highlighted by the “Rule of the Hand” can do much to avoid the problems of diabetes, and lead to a better quality of life.
Dr. Stephen A. Wilson, MD, MPH, FAAFP, is Chair of Family Medicine at Boston University Chobanian and Avedisian School of Medicine, Chief of Family Medicine for Boston Medical Center, President of Boston University Medical Group - Family Physicians, Inc., and a member of the ENC Board of Trustees.